Technical Challenges of Percutaneous Transhepatic Biliary Drainage in Adult Biliary Atresia Patients Post Kasai Portoenterostomy
DOI:
https://doi.org/10.3941/jrcr.5473Abstract
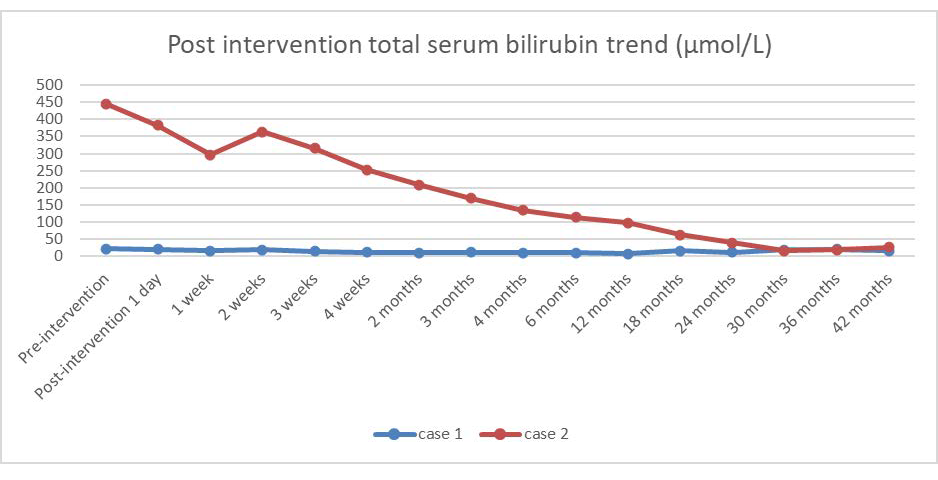
Biliary atresia (BA) is a severe hepatobiliary condition requiring Kasai portoenterostomy (KP) during infancy to facilitate biliary flow. However, post-KP, patients frequently develop complications such as recurrent cholangitis, biliary stricture, and cystic intrahepatic dilatation. These complications often progress to biliary cirrhosis and end-stage liver disease, necessitating liver transplantation.
In this context, we explore the application of Percutaneous Transhepatic Biliary Drainage (PTBD) for treating biliary complications in post-KP BA patients. PTBD in these cases is technically challenging due to the presence of biliary strictures and intrahepatic bile duct dilatation, and its effectiveness has been a subject of debate.
This paper presents two technically challenge cases where we treated adult BA patients who developed late-onset biliary strictures following successful KP. Both of the required first direct puncture of a cystic region of biliary dilatation, followed by successful puncture (one patient was punctured on CT-guidance) and wire cannulation and successful PTBD insertion. Following the procedure, both patients achieved short-term and long-term clinical improvement. The significant findings from these cases include: resolution of acute cholangitis, normalization of liver enzymes, no evidence of biliary cirrhosis in subsequent ultrasound, and removal of both patients from the liver transplantation list.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Journal of Radiology Case Reports

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The publisher holds the copyright to the published articles and contents. However, the articles in this journal are open-access articles distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 License, which permits reproduction and distribution, provided the original work is properly cited. The publisher and author have the right to use the text, images and other multimedia contents from the submitted work for further usage in affiliated programs. Commercial use and derivative works are not permitted, unless explicitly allowed by the publisher.